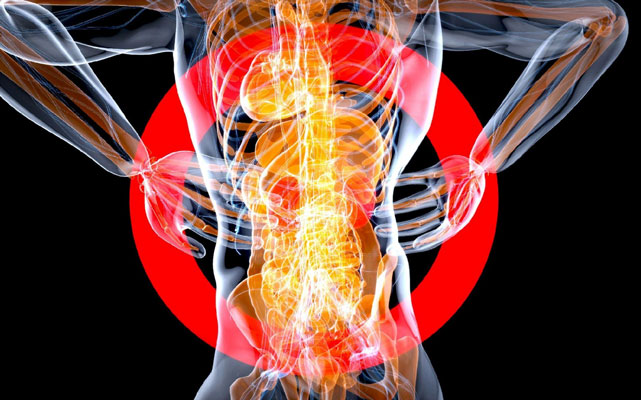
Back pain is such a commonly shared experience that it’s difficult to know when specialist care is needed.
It’s easy to attribute symptoms to simply sleeping in an uncomfortable position, standing for too long, or bending over too much from gardening. In many cases, it’s true, and symptoms may go away after a few days of rest and some OTC anti-inflammatories.
If your pain lasts longer than a few days, despite taking proper care of yourself, that’s your first clue that your pain may not be what it seems. It could be due to a more complex issue with your nerves, bones, or soft tissue. In some cases, persistent back pain is a sign of a deeper neurological health problem.
Here are more signs that it’s time to see a specialist.
Talk to Your General Physician
If your back pain becomes noticeably stubborn, despite your best efforts, book an appointment with your doctor to be on the safe side.
At this time, log all of your pain symptoms, including times of day, in a journal. Leave no stone unturned, since back pain can be a symptom of various issues.
Talk to your doctor about steps taken to lessen the pain, like limiting certain activities, rest, OTC medications, and proper footwear.
Remember, your general physician is the first “stop” on the route toward specialist care. They’re the one who refers you to a specialist for further diagnostic testing and treatment.
Monitor the Situation for 6 Weeks
After an initial appointment, your doctor may recommend physical therapy to see if symptoms improve. This recommendation may also include heat therapy and ice-packing.
Monitor the situation for about 6 weeks to see if there are any changes in your symptoms. Acute back pain is a musculoskeletal issue and often resolves itself within a month with proper at-home care.
If symptoms persist past this mark, touch base with your doctor for next steps. This could result in a specialist referral for a physiatrist, orthopedic surgeon, or neurosurgeon. A specialist can use diagnostic methods to see if you have a degenerative disc or spinal stenosis, for example.
When Pain Moves Beyond the Back
If your pain is spreading to other parts of your body, that’s cause for concern. This could mean a deeper issue with your nerves.
Radiculopathy is one such issue. A specialist can investigate if the nerve root in your spinal column is compressed or inflamed. Rather than a standard backache, radiculopathy pain is sharp with almost shock-like sensations. You may experience tingling or numbness in the arms and legs, as well.
Back pain can be a sign of neurological weakness, especially when it’s accompanied by stumbling or difficulty with lifting the front of your foot, known as foot drop. Saddle anesthesia can also occur, causing numbness in your inner thigh area.
Can Back Pain Become an Emergency?
If back pain is accompanied by loss of bowel or bladder control, that’s an emergency. It could be a sign of Cauda Equina Syndrome, which requires emergency surgery. This condition results from nerve root compression in the spinal cord.
Cauda Equina Syndrome may also be caused by a tumor, fracture, herniated disk, or another form of spinal nerve compression.
When Should You Get a Microdiscectomy?
If you have a herniated disc in your lower back, a specialist may recommend a microdiscectomy to remove the herniated part that’s compressing the nerve. It’s also possible to have a herniated disc in the neck, which requires a cervical microdiscectomy.
Microdiscectomies are minimally invasive procedures with relatively fast recovery times. Patients experience quick nerve pain relief, but it takes some time to enjoy full pain relief.
It’s typically a same-day procedure that allows patients to go home the very same day. Patients are advised to rest for at least two weeks before gradually resuming normal activities. However, strenuous activities, like heavy lifting, should be avoided for at least six weeks.
Patients may begin physical therapy after six weeks or when advised by the specialist. Rebuilding back and neck strength is essential for mobility and preventing long-term chronic pain.
What Is the Role of Diagnostic Imaging?
Some back pain cases may require an MRI. A specialist may order an MRI if you’re still experiencing significant back pain after 4 to 8 weeks of physical therapy. An MRI will provide more clarity into potential soft tissue damage, as well as compressed nerves and herniated or ruptured discs.
If you experienced an accident, like a car crash or fall, a physician will immediately order an X-ray or even a CT scan to check for spinal bone fractures or other injuries that require quick stabilization.
When Does Back Pain Become Chronic?
Back pain is typically considered “chronic” if it lasts for more than three months. However, there are still options for relief and restoration.
A specialist can recommend interventions like surgeries and clinical pain management methods like epidural steroid injections. The goal is to reduce inflammation as much as possible.
Listen to Your Back Pain
Back pain can be easy to ignore, especially with the realities of life and work. But if your pain grows increasingly stubborn, don’t ignore your gut instinct that something is wrong.
Allow yourself a couple of weeks to rest and slow down to see if that helps. If you’re still in pain, talk to your doctor about the best course of action. Severe cases of back pain may need medical interventions like surgery, injections, or physical therapy.
Create a life that’s free from back pain.